Renal system
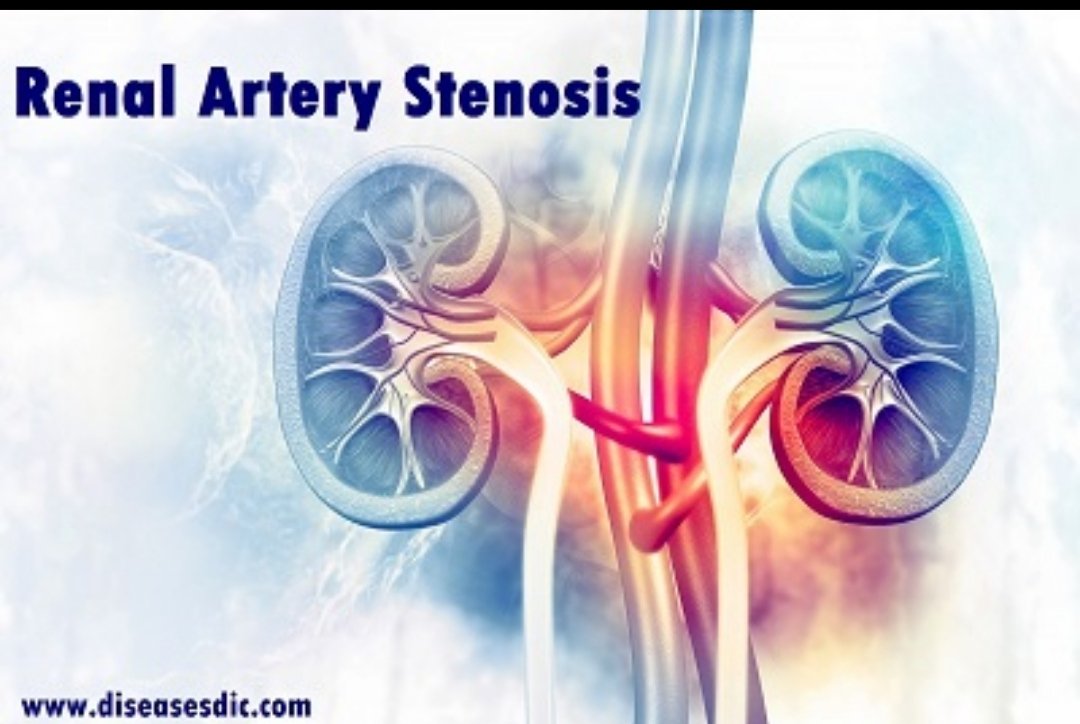
renal artery disease or kidney stenosis) occurs when the two main vessels that deliver blood to the kidneys become stiff or narrowed due to vascular disease. RAS is a type of atherosclerosis or hardening of the arteries, which occurs when fatty cholesterol plaques build up inside artery walls. The kidneys perform several key functions in the body, including regulating blood pressure and removing waste and toxins from the blood. Renal artery disease can reduce the amount of blood that’s able to flow into the kidneys, which can raise blood pressure and allow toxins to build up in the body’s tissues. This condition may often lead to renal failure.

Pathophysiology
RAS is primarily caused by atherosclerosis, or clogging, narrowing, and hardening of the renal arteries. In these cases, RAS develops when plaque builds up on the inner wall of one or both renal arteries, making them hard and narrow.
Renal blood flow is three to four times greater than the perfusion to other organs due to the need to perform glomerular filtration. In patients with RAS, the chronic insufficiency produced by the obstruction of renal blood flow leads to kidney changes that are more pronounced in the tubular tissue. These include inflammation, fibrosis, tubulosclerosis, and intrarenal arterial thickening.
In patients with RAS, when renal perfusion pressure drops below 70 mmHg to 85 mmHg, the autoregulation system between the afferent and efferent arteries can fail to maintain the glomerular filtration rate (GFR). This will lead to a decrease in the GFR, but will not likely be observed until arterial luminal narrowing exceeds 50%.
There is currently no formal recommendation for when to intervene surgically or radiologically in RAS. It is reported that a ratio of pressure less than 90%, measured distal to renal artery stenosis relative to aortic pressure, was associated with significant renin release from the affected kidney. This might be useful as a functional measurement of significant renovascular stenosis leading to hypertension and, thus, a marker of a greater likelihood of benefit from angioplasty and stenting.
The other main cause of RAS is fibromuscular dysplasia (FMD) the abnormal development or growth of cells on the renal artery walls which can cause blood vessels to narrow.
Renal artery stenosis risk factors
There are a variety of factors that could put you at risk for developing renal artery stenosis; the most common are:
Atherosclerosis
Advanced age
Diabetes
Gender – women are at higher risk
High cholesterol
Hypertension, particularly new onset of hypertension in an older person
Smoking
Keep in mind that although these factors increase a person’s risk, they do not necessarily cause the disease. A patient with several of these risk factors may never develop the disease, while others with no known risk factors may develop the disease.
Causes of Renal artery stenosis
Atherosclerosis (hardening of the arteries) causes renal artery stenosis. Atherosclerosis occurs when plaque builds up on the artery walls, narrowing them and slowing blood flow. Factors that increase your risk for atherosclerosis include:
Smoking
High blood pressure
High cholesterol
Obesity
Family history of heart or vascular disease
Symptoms
Renal artery stenosis often doesn’t cause any signs or symptoms until it’s advanced. The condition may be discovered incidentally during testing for something else. Your doctor may also suspect a problem if you have:
High blood pressure that begins suddenly or worsens without explanation
High blood pressure that begins before age 30 or after age 50
As renal artery stenosis progresses, other signs and symptoms may include:
High blood pressure that’s hard to control
A whooshing sound as blood flows through a narrowed vessel (bruit), which your doctor hears through a stethoscope placed over your kidneys
Elevated protein levels in the urine or other signs of abnormal kidney function
Worsening kidney function during treatment for high blood pressure
Fluid overload and swelling in your body’s tissues
Treatment-resistant heart failure
Renal artery stenosis complications
People with RAS are at increased risk for complications resulting from loss of kidney function or atherosclerosis occurring in other blood vessels, such as
Chronic kidney disease (CKD)- Reduced kidney function over a period of time
Coronary artery disease- Narrowing and hardening of arteries that supply blood to the heart
Stroke- Brain damage caused by lack of blood flow to the brain
Peripheral vascular disease- Blockage of blood vessels that restricts flow of blood from the heart to other parts of the body, particularly the legs
RAS can lead to kidney failure, described as end-stage renal disease when treated with blood-filtering treatments called dialysis or a kidney transplant, though this is uncommon in people who receive ongoing treatment for RAS.
Diagnosis and test
You will be asked questions about symptoms and medical history, including questions about family members. Your vascular surgeon will also perform a physical exam that may include placing a stethoscope on your abdomen to listen for signs of abnormal blood flow.
Tests may be recommended
Duplex ultrasound uses high-frequency sound waves to measure real-time blood flow and detect blockages or other abnormalities in the blood vessels.
Magnetic resonance angiography (MRA) uses magnetic fields and radio waves to show blockages inside your arteries.
Computed tomographic angiography (CTA) uses specialized CT scans and contrast dye to show blockages inside your arteries.
Angiogram produces X-ray images of the blood vessels with the help of a contrast dye that highlights your arteries. This is usually recommended only for patients needing treatment of renal artery stenosis using catheter-based techniques.
Treatment and medications
Treatment is dependent on your overall health and the symptom experienced, but usually involves lifestyle changes, medication, or medical procedures. Oftentimes a combination of these therapies is the best option for management. Lifestyle modifications would include quitting smoking, trying to maintain a healthier weight, and getting regular exercise such as walking at least 30 minutes, 3 times a week. Also, it is very important to control other risk factors, by taking the appropriate prescribed medications to control blood pressure, cholesterol, and diabetes.
Medications prescribed by your vascular surgeon may include:
ACE inhibitors or ARBs: Helps relax your blood vessels and block the effects of a naturally occurring body chemical called angiotensin converting enzyme II, which narrows blood vessels
Diuretics: Help eliminate excess water from the body
Beta blockers: make your heart beat slower and more effectively, and can widen and dilate the blood vessels
Calcium channel blockers: Relaxes blood vessels
Statin drugs: These will help keep your cholesterol levels better controlled, preventing further plaque build-up in your arteries